FSGS
The classic podocytopathy
- Huge aetiology for a relatively generic pathological pattern
- Podocyte- 300-500 per glom in humans, don’t regenerate well
- Pod depletion is central to the disease process – death, senescence,
apoptosis ->podocytopaenia -> glomerlular sclerosis
- During pod injury -> misdirected filtration -> adhesion of the
tuft to bowmans capsule ->progressive adhesions and scar
- In animal models the podocyte depletion correlates with proteinuria
and glomerular sclerosis
- Seems there’s a threshold of maybe 20% of depletion before series
disease kicks
- On a spectrum of disease alongside MCD?
Primary FSGS
- Classic presentation – microscopy of the kidney biopsy demonstrates
FSGS lesions, electron microscopy of the kidney biopsy demonstrates
diffuse foot process effacement, and clinically the patients display
nephrotic syndrome.
- No other obvious cause of FSGS
- Circulating factor? – supar- beta3integring?
- Cardiotrophin-like cytokine 1
- IL6 family
- Returns after tx, Savin 2006(?96) NEJM- 33/56 tx’d recurred – PEX
reduced the glom permeability to albumin here
- Classic NEJM 2012 resolution of recurrent FSGS when a failing
“recurrent FSGS” was tx’d into a second patient
- Low serum alb
- Bx: collapsing, tip lesion, NOS are all common
- On the EM – foot process effacement, in contrast to secondary
forms
- Steroid sensitive or dependant. Responsive to IS – if not improving
consider if secondary and screen
- Steroids: 1mg/kg, max 80mg, 16-week max trial, if respond give
>=6 months. CNI/cyclosporine alternative
- Spontaneous remission rates are >20%.
- NS have worse kidney prognosis than non-nephrotic patients, with
10-year kidney survival rates of 57% compared to 92% in those with lower
degrees of proteinuria
- Response of proteinuria predicts outcome Troyanov JASN 2005
- 40% don’t response to steroids – only 20% renal survival in this
group
- Adults with FSGS who do not have nephrotic syndrome should be
evaluated for a secondary cause
Maladaptive
- Glom load>capacity – hyperfiltering and stretching podocytes
- Unilateral renal agensis, hypoplasia
- Renal ablation
- Obesity
- Absolute unit
- Extensive nephron loss from other diseases e.g. GN
- Oligomeganephronia
- Typically normal albumin, but can have nephrotic range
proteinuria
- May lack oedema
- Large body size ?Premature birth
- Bx: large gloms, glom scars tend to perihilar (>-50%)
- Often responds to conservative therapy – ACEi/ARB low dose thiazide,
NA restrict
- Lose weight, stop anabolic steroids
APOL1 FSGS
- Serum lytic for T.b.Brucei. G0/G0 susceptible. G1/G2(or G2) risk of
CKD.
- Single allele may be enough to increase risk/trigger FSGS
- Diseases tend to progress faster if homozygous
- Fertile soil hypothesis: Podocytes (maybe vascular cells) are more
susceptible to injury due to altered endolysomal function or
inflammatory signalling
- Gorillas have risk alelles, chimps don’t. mice don’t.
- Aboriginal Australians likely don’t as they arrived in Australia
50000 years ago after an African migration 72000 years ago. It is
thought the APOL1 G1 and G” arose in sub Saharan Africans only about
5000-10000 years ago. ( https://www.kidney-international.org/article/S0085-2538(17)30086-8/fulltext)
- 72% west African/sub–Saharan FSGS
- Can manifest in various ways due to additional factors: Associated
with HIVAN, aterionephrosclerosis (misattributed to HTN perhaps), sickle
cell (RR3.4), prematurity, drug induced (interferon),eclampsia (RR
1.6)
- Transplant: Risk in donor genotype (HR 3.8) ( no effect in
recipient)
- Seems to explain about 75% of HIVAN and even much of “primary” FSGS
in case control studies
- No different in steroid sensitivity between APOL1 risk
alleles vs G0
- No meaningful change in response to therapy
Genetic FSGS
- Up to 20% of steroid resistant FSGS patients ( yaeo et al CJASN
2019) – about 55% col4a3/4/5, 40% podocyte and 5% CAKUT genes
- Mendelian AR AD
- Mitochondrial
- X-linked
- Typically slit diaphragm/podocyte defects
- Family hx/ consanguinity
- Extra renal manifestations – skeletal, neurological, eye, ear,
urogenital
- Why – might help prognosis and hunt for extra-renal manifestations,
transplant and family implications, family closure
- Acetyl Q10 in some diseases – worth checking
- Steroids generally don’t work, CNI’s might
- Good Conservative care vital
- Whole exome sequencing probably overtaking the panels
Virus
- HIV = interferon drives APOL1 gene expression
- CMV- collapsing FSGS
- Parvo b19?
- EBV?
- Simian virus 40
- Hepatitis C
- SARS-COV 2 ( with APOL1)
Meds
- Interferon – drives APOL1 gene expression
- Bisphosphonates - collapsing
- lithium – primary phenotype
- CNI - adaptive
- Amphotericin
- Heroin
Misc
- Cholesterol crystal embolization
- Renal artery stenosis
- Rejection
- Aging
- Congenital cyanotic heart disease
Treatment
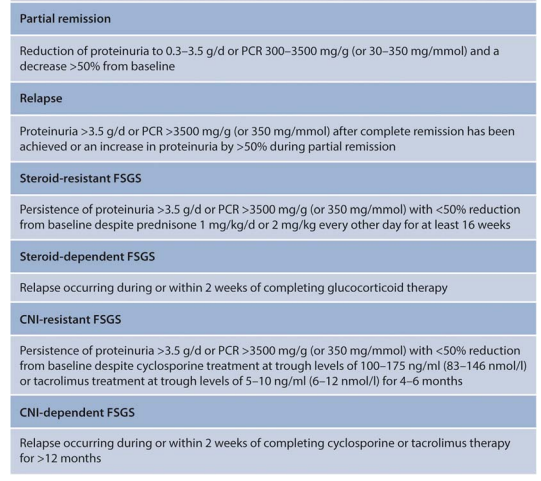
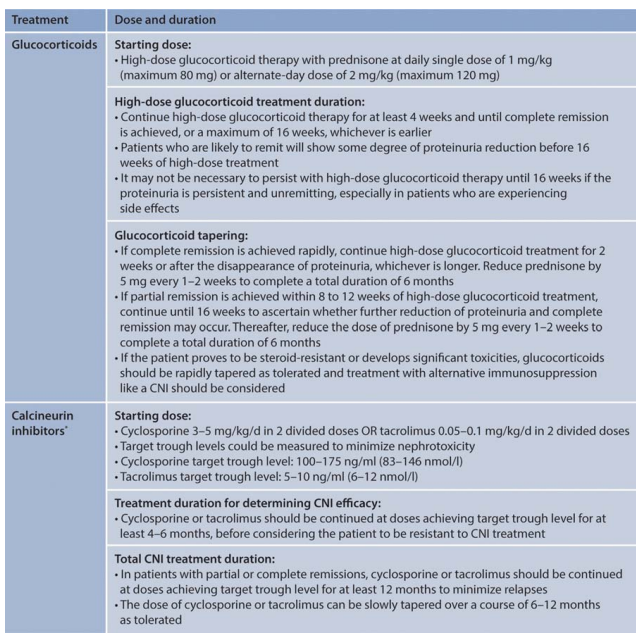
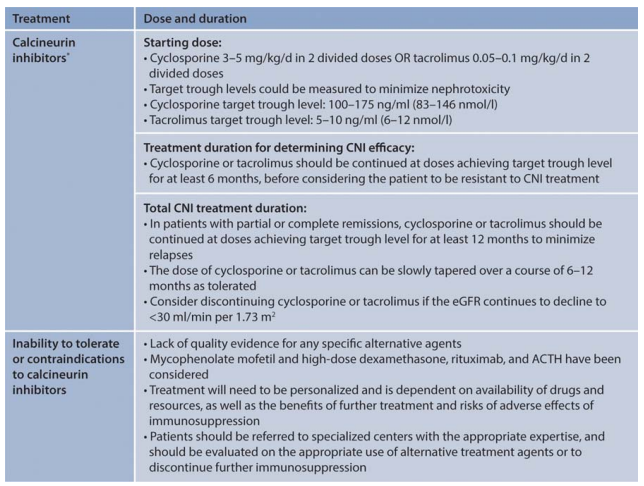
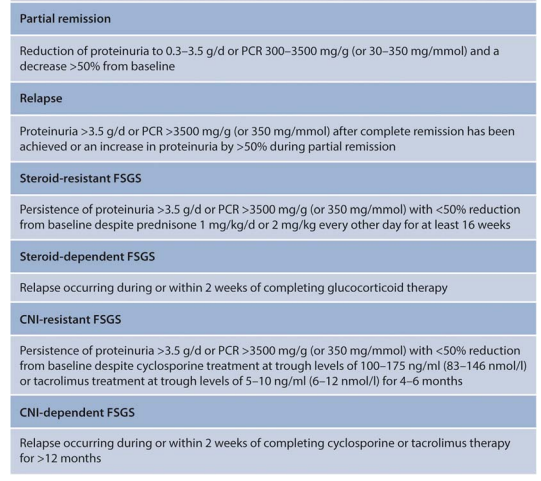
figures from KGIDO GN 21
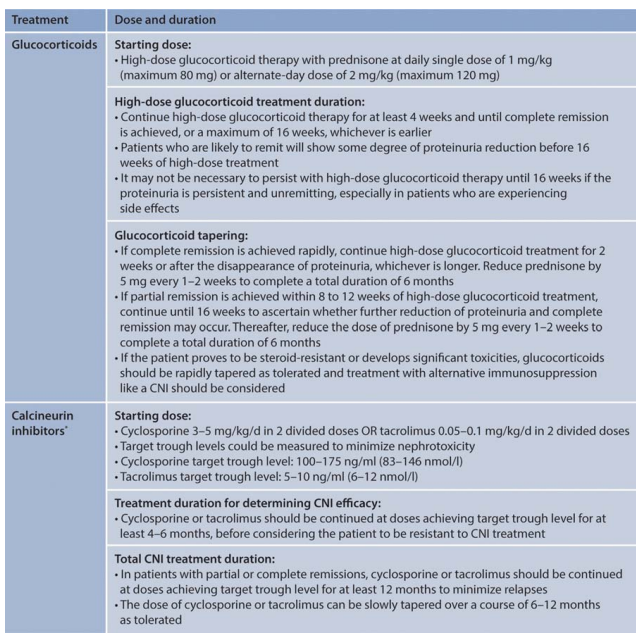
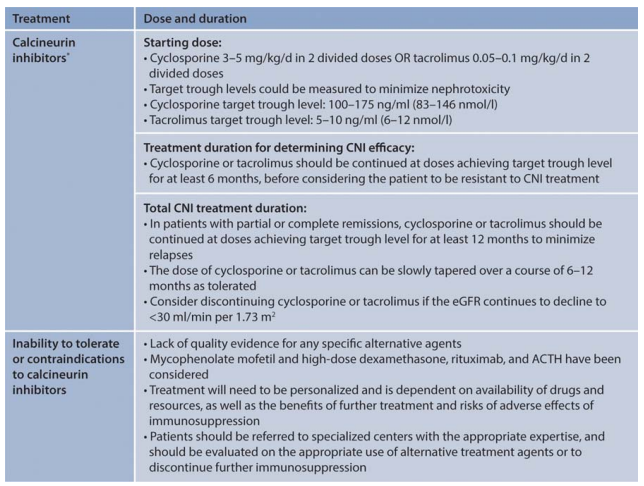
Rx Notes
- Podocytes love steroids, seems to strengthen the cytoskeleton
- CNI (nat med 2008 Faul,C) – stabilises synaptopodin
- ?voclosporin
- Rituximab – appears to stabilised podocyte membrane also (ravani et
al CJASN 2016)
- Sparsentan – Endothelian1/ARB – DUET – decreased proteinuria, phase
3 ongoing
- CCR2 antoagonism
- Abatacept in B7-1 prositive proteinuric kidney disase 9 NEJM13
- VEGFr is an attractive signalling pathway as is TGFB-TGF-R1 ( could
my drug work here?)
Steroid subtlties
Glassock on the ASN forums:
This discussion would not be complete without a critique of how we
(arbitrarily) define resistance to steroid therapy in apparently Primary
FSGS in Adults. The group in Nijmegen, Netherlands have added some
important information to this quandary . Prolonged steroid therapy (well
beyond the time used by KDIGO to define ’steroid resistance ” can be
beneficial long term especially if there is an early decline in
Proteinuria of > 20% from baseline ( see Rood UM, et al KI Reports
2022; 7: 87-92). Also , in those who experience a partial or complete
remission with steroids early in the course, maintenance of the
remission can be crucial for long term benefits. ( see Jauhal A, et al
NDT, August 10,2022).
Resistant FSGS
Per Glassock on the ASN forums
misc - compile and order later
https://jasn.asnjournals.org/content/29/3/759
primary vs secondary cause
nephrotic syndrome vs nephrotic range proteinuria
While not 100% in most cases, nephrotic syndrome and FSGS usually is
going to have a primary cause( sparing some genetic causes and viruses).
In addition, what is also helpful from a pathology standpoint is not the
LM, but the EM–
- Is there diffuse or partial foot process effacement?- Usually the
former responds to treatment better with steroids or other
immunosuppression and later is more likely a secondary cause. It may
also aid in looking for a secondary cause.
Classically, your “permeability or immune mediated” FSGS should
respond to treatment and would fit under nephrotic syndrome, diffuse
foot process effacement and classically your primary FSGS. Secondary
FSGS from various causes like low nephron mass, obesity, viral , meds-
all classically would have nephrotic range proteinuria and sporadic foot
process effacement on EM.
no one really knows what is the optimum approach to such
patients. Desparate but unproven measures are commonly undertaken- such
as the “kitchen sink” regimens of multi-target therapy or PLEX/lipid
Apheresis. dramatic effects can be seen (anecdotes) but impossible to
predict.
ESKD and dialysis dependency are common no matter what is done,
in most cases.
the risk of recurrent disease in the allograft is very high, if a
genetic disease is excluded
the role of repeat biopsy is completely unknown, although it
might be used to declare futility or to enhance the likelihood of CNI
toxicity in selected patients.
progressive elevations of serum creatinine suggest a poor outcome
, except when CNI is strongly suspected . Regimens including CNI are
potentially hazardous in such patients .
referral to a Center of Excellence for consideration of
enrollment in an ongoing interventional trial should be strongly
encouraged.
KDIGO: FSGS-UC (for undetermined cause). It is conceivable that
patients with FSGS-UC have secondary or genetic forms of FSGS that have
not yet been elucidated
FSGS –histological variants – unsure how useful this really is
clinically
- Collapsing
- Perihilar
- Cellular
- FSGS NOS
- Garbage bag of everything else
- TIP variant
May have segmental scar (classic, tip and perihilar) which can be
missed and misdiagnosed as MCD – these can often be later reclassified
as “presumed FSGS wen the patient doesn’t get better)