- Minimal Change Disease
- Typical Steroid Course
- Relapse
- Anti-Nephrin antibodies
- Mintac
- Key Papers
Minimal Change Disease
- ~10-15% of NS
- 30-50% can remit without treatment but may take up to 2 years
- Probably can progress to FSGS
- Over 80% of adults with MCD are steroid responsive.
- 50-70% of adult patients will relapse
- 1/3 patients may become frequent relapsers or steroid dependent Waldman et al, cJASN 2007.
- Rapid onset of nephrotic sydrome
- 15% of adult cases are secondary: nonsteroidal anti-inflammatory drugs, lithium, and lymphoproliferative disorders
- Hypertension (25%–50%), hematuria (20%–30%), and AKI ( ATN? )(20%–25%) are more common in adults
- Rarely can lead to CKD, or even ESRD ( <5%)
- Anticoagulation: lower risk but perhaps if resistant?
Typical Steroid Course
- Remission in ~50% adults by 8 weeks, 75-95% by 16.
- 1mg/kg, max 80mg po od - 4 weeks minimum, up to 16 weeks if waiting on remission
- Run 2-4 weeks post remission
- Reduce to achieve total treatment of 4-6 months
- Remission is classically quite abrupt
Relapse
- Common, 65-80%
- Usually first 3-6 months post remission
- Age <45 relapse more (?better immune system?)
- 1st relapse - repeat pred course
- 2 * courses in 6/months or 4/12 = frequent relapser
- 10-30% are frequent relapses and 15-30% are steroid dependant
- Probably reasonable to give ritux although weight of evidence us for cylophos. Ruggenenti et al JASN 2014
- RTX (4 weekly doses of 375 mg/m2
- Cyclophos po ~2mg/kg po od * 8-12 weeks. ( note dose adjusted by age & eGFR)
- Partial remission is rare - rebiopsy for missed FSGS on bx?
Anti-Nephrin antibodies
Heres a pretty good freely filtered where the author Astrid Weins is interviewed - really enlightening ideas. Some conceptual highlights included
- Fine granular IgG dusting on almost all MCD bxs !?
- MCD-FSGS spectrum
- ~30% of MCD disease have circulating anti-nephrin antibodies (NEPTUNE cohort)
- Anti-nephrin is basically the perfect assault molecule vs slit
diaphragm.
- IgG is freely filtered - just zooms past the slit diagram, is continually replenished, hours of affinity perhaps, and it gets instagibbed. Slit diaphragm integrity disrupted.
- Doesnt need to accumulate and cause immune complexs( unlike anti-PLAR2)
- The antibody/antigen balance is probably very subtle and minor effects will shift clinical picture ( steroids etc)
- Fastest responders seem to loose ab over days.
- No antibodies in patients in remission.
The pathology of acute nephrotic syndrome in MCD
- Effacement = nothing goes through = higher pressure
- disrupted structure results in Bigger pore size
- Nephrotic syndrome ramps up the pressure and overcomes the negative charge of the endothelium which allows negative albumin.
- Therefore dont need to alter endothelium, just need to overcome it via ramping up pressure/pore size ( ?via nephrin -> actin cytoskeleton disruption)
Recurrance post tx
Rare. not sure how this fits with FSGS high recurrance.
Adult data here **
In rare cases Recurrance post tx of congenital nephrotic syndrome is thought to be driven by anti-nephrin abs ( and responds accordingly to b-cell depletion) re paediatrics, in congential (primary is typically AR vs NPHS1(nephrin)/NPHS2) nephrotic syn and tx:
- Recurrance is rare in congential forms
- Return of proteinuria is common in non congenital forms (80% of total)
Mintac
The mintac trial
- Oral tacrolimus at 0.05 mg/kg twice daily vs or prednisolone at 1 mg/kg daily up to 60 mg daily.
- The primary outcome was complete remission of nephrotic syndrome after 8 weeks of therapy.
- Secondary outcomes included remission of nephrotic syndrome at 16 and 26 weeks, rates of relapse of nephrotic syndrome, and changes from baseline kidney function.
Mintac Protocol
- Everyone got Acei, statin (if required)
- Run tacro levels 6-8
- At week 8, if inadequate clinical response, target blood trough level was increased to 9-12 ng/ml.
- 12 weeks after achieving complete remission, tacrolimus doses were
titrated down over 8 weeks and stopped.
- Participants in prednisolone arm received an initial dose of 1mg/kg per day with a maximum dose of 60 mg/kg per day.
- One week after achieving complete remission, the steroid dose was halved for 4-6 weeks then gradually reduced and stopped over a further 6 weeks. Patients received a minimum of 16 weeks prednisolone. Bone and gastric protection was with calcium carbonate/cholecalciferol (1000mg/800IU) two tablets daily and omeprazole 20mg daily
- Complete remission was defined as uPCR <50 mg/mmol
- Results non inferior
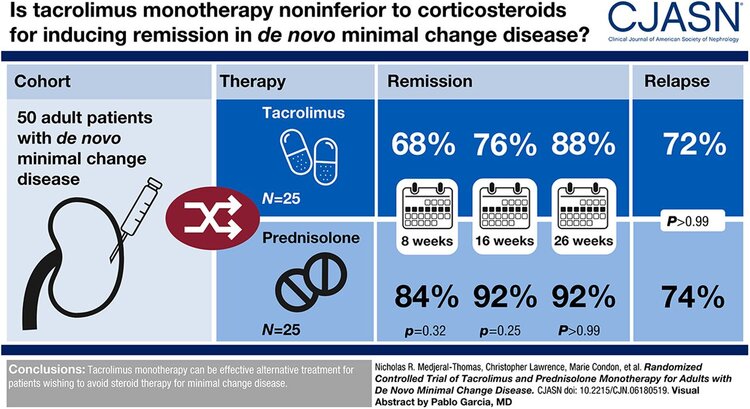
abtract by Pablo Garcia
Key Papers
Nature reviews Nephrology: MCD-FSGS spectrum
- Early FSGS must have some early podocyte injury - some believe this is the same intial injury and FSGS is end game
- Genetic / environmental factors
CJASN: nice review on clinical features of MCD