- MPGN
- Histology
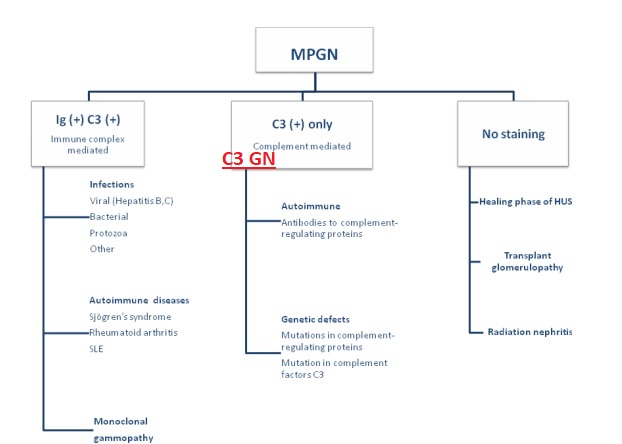
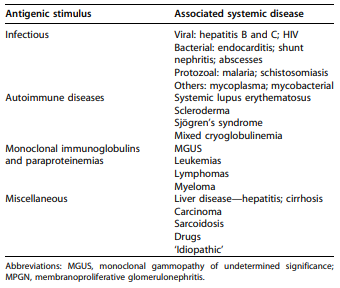
- Classification
- MPGN Treatment
- MPGN Outcomes
- IGAN & MPGN
- C3G
- G3G Treatment
- C3G Outcomes
- Misc tips
MPGN
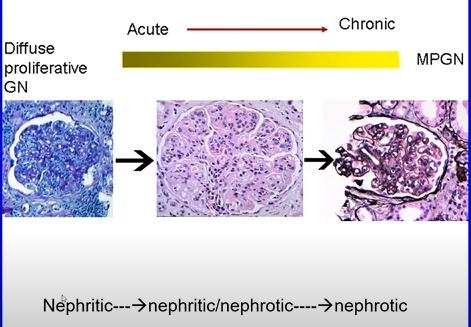
Chronic deposition of debris along the glomerular capillary walls which leads to inflammation.
MPGN is a pattern of injury – diverse aetiology
The deposits can be Ig, complement, fibrin
Glom responds to injury, tries to heal/wall off insult with addtional GBM, creates double contours / tram-trak
Very important to clarify is this is an Ig related disease (more treatable) vs C3G (complement dysregulation, more challenging treatment, worse outcomes)
Histology
Light microscopy
- Two features – inflammation and healing
- Inflammation is the “proliferative” phase – MPGN – Mesangial and endocapillary hypercellularity
- Resolving/healing phase – MPGN - mesangial expansion with matrix and thickened capillary walls, cellular interposition with double contour formation
Immunofluorescence
- Immunoglobulins, Kappa or Lamda light chains, C3
Electron microscopy
- Mesangial deposits, capillary wall deposits (sub endothelial), cellular interposition and new basement membrane formation – ie. double contours
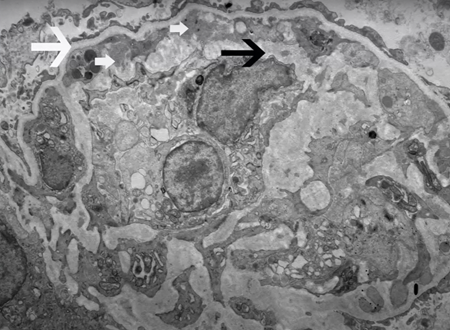
Small White arrows – sub endothelial deposits. Basement membrane is trying to “trap” the deposits as a reaction, just like an abscess being formed and walled off. Incoming cell inflammatory cells (monocytes) get “interposed”
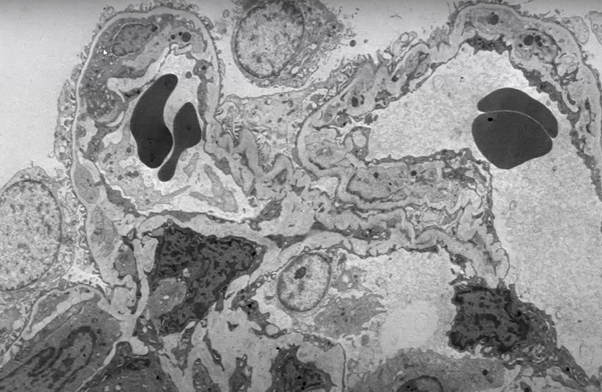
More classic appearance here, note entire cell on the left is entrapped, and debris on the right. (images from the Glomcon episode of Sanjeev Sethi, MD, PhD Professor Department of Laboratory Medicine and Pathology Mayo Clinic Rochester, USA Glomcon
Classification
Immunofluorescence/aetiological classification has replaced the older typing, is often much more informative than as allows more meaningful subdivision
~75% are down the left side typically and Ig associated. In the case of Ig positive on IF, then run through a list of differentials similar to this -
MPGN “traditional classification” - based on EM, disregarded IF.Not very useful, historical interest mostly. Confusing. Ignore.
Primary:
- Type 1 sub endothelial
- Type 2 AKA dense deposit disease - intramembranous
- Type 3 subendothelial, intramembranous and subepithelial
Secondary:
- Infection, Hep C was classic
MPGN Treatment
MPGN Outcomes
IGAN & MPGN
- Association with chronic liver disease - often with infection, occult ~(42%)
- At 7 weeks, 80% died - agressive variant
- Non liver disease patients, 73% men, age 40. 27% ESKD by 3 years.
C3G
All ages, no sex predilection
Nephritic -> nephrotic presentation
Typically, present with HTN, proteinuria and haematuria
Bright C3, minimal or no Ig - typically 2 orders of magnitude higher than the background Ig staining
2 flavours C3GN, DDD (EM)
Usually shows MPGN but other patterns possible e.g. “post infectious”
if coexisting IG, more likely to have an autoantibody rather than infection
C3GN When associated with infection
Some of these have very distant infections which might be associated with complement mutations or residual auto antibodies
G3G Treatment
If associated with Ig/MRUS – clone directed treatment
Haematological remission gives best chance of good renal outcomes and evidence suggests good outcomes
https://pubmed.ncbi.nlm.nih.gov/29759418/
Excluding the monoclonal related disease then IS seems ineffective
C3G Outcomes
50% hit ESKD in 5 years
Usual suspects predict outcome: fibrosis, tubular atrophy, High presenting Cr, proteinuria >3g/24 hours
Misc tips
The renal bx and bone marrow dont match? (e.g. you suspect MPGN from K/L light chains based on marrow but arnt seeing that on the renal bx) - request a paraffin-IF with Pronase digestion and a stain with Heavy-Light chain hybrid antibody to sub-type the IgG - immuno-gold EM to see if the electron dense deposits are composed of a monoclonal light chain.