Hyponatreamia
Hyponatraemia is all about ADH typically
Isothenuria normal in aging and in AKI/CKD.
- Urine diulation is active and difficult
- Normal adult can generate dilute urine - 50mOSM/Kg
- “Normal” diet is 10mOSM/kg/day, so 70kg male = (10*70)=700/50(daily limit)=14litres
- Elderly limit ~150 mOSM/kg. Diet intake can be low (tea and toast) e.g. (3*50)/150=1Litre/day. free water over this limit dilutes urine.
Hypotonic hyponatraemia requires treatment (probably), so confirm a pOSM if possible.
k+ is oncotic too ( and can buffer NA) - 20mmol/KCL = 40ml 3% NaCL - may overcorrect if not aware!
Urine Na: >30 mmol/l urinary Na = dry (NB low [Na] diet, diuretics, CKD - poor reabsorbtion (and impaired free water clearance too))
Urine Osm: <100 mmmol/L = appropriately dilute. 100 - serum osm = grey area.
- Remember that a measured osm also measures ineffective osmolues such as Urea or Ethanol - may be artefactually high and mask true hypoosmolar state
Non-hypotonic (hyperglycaemia, mannitol, hypertonic radiocontrast,pseudohyponatreamia) - conservative Rx
Correction
- Hypertonic Saline: 3% 150 mls/20 mins. recheck while giving second bag. target increase of 5mmol/L
- 0.9% Saline = 154mmol/L, 3% Saline =513mmol/L
- 1ml/kg/hr 3% NaCL corrects Na ~ 1mmol/l/hr. e.g. 70mls/hr =1. so 150mls = ~2ish.
- Speed limit: 10/first 24 hrs, 8/24 hrs thereafter
- Fix overcorrection with a DDAVP clamp as below: 5% glucose and DDAVP 2/4mcg sc as below
- Once stable - give 3% saline as follows, remembering to substract bolus:
6*(Totalbodywater+1)/(513-initial NA) = total volume - boluses already given. Divide by hours (typically 4). HDU and monitor every 4-6
Osmotic demyelination
Risks: Female, hypokalaemia, chronicity, alcoholism, cirrhosis, malnourishment.
Pseudohyponatreamia
Triglycerides, cholesterol, or protein
Hyperglycaemia correction of Na
This translates into adding 2.4 mmol/l to the measured serum sodium concentration for every 5.5 mmol/l (100 mg/dl) incremental rise in serum glucose concentration above a standard serum glucose concentration of 5.5 mmol/l (100 mg/dl). (Ive seen this as 1.6mmol/L also)
Free water clearance
Useful conceptually (in chronic state), not very quantitativly, and inconvienient outside ITU
Calculation
cH2O = uV - (uOsm x uV)/pOsm
where cH2O = Free Water Clearance
- where uV = Urine Volume per unit time ( make it a day I guess if 24 hours collection)
- where uOsm = Urine Osmolality
- where pOsm = plasma osmolality
Interpretation
Free Water Clearance positive
Urine less concentrated than plasma
Decreased Antidiuretic Hormone (ADH) Free Water Clearance negative
Urine is more concentrated than plasma
Increased Antidiuretic Hormone (ADH)
SIADH criteria
SIADH is pretty rare. Be suss.
Essential criteria
Effective serum osmolality >275 mOsm/kg
Urine osmolality >100 mOsm/kg at some level of decreased effective osmolality
Clinical euvolaemia
Urine sodium concentration >30 mmol/l with normal dietary salt and water intake
Absence of adrenal, thyroid, pituitary or renal insufficiency
No recent use of diuretic agents
Supplemental criteria
- Serum uric acid >0.24 mmol/l (>4 mg/dl)
- Serum urea >3.6 mmol/l (>21.6 mg/dl)
- Failure to correct hyponatraemia after 0.9% saline infusion
- Fractional sodium excretion >0.5%
- Fractional urea excretion >55%
- Fractional uric acid excretion >12%
- Correction of hyponatraemia through fluid restriction
Desmopressin aka DDAVP
In DI: If intravenous saline solution is administered and desmopressin is withheld at the same time, rapid changes in serum sodium levels may result, which puts the patient at risk for demyelinating lesions.
- Opinion: In the management of desmopressin-associated hyponatremia with neurologic symptoms, the drug should not be withheld despite the presence of hyponatremia. Instead The medication should be continued while administering intravenous hypertonic saline solution.
DDAVP Clamp: Desmopressin is also used to minimize water excretion during the correction of hyponatremia during water diuresis. When treating hyponatremia, clinicians should monitor closely to avoid free-water diuresis. To prevent ongoing water losses in urine and overly rapid “autocorrection” of serum sodium level, desmopressin can be given to reduce free-water losses.
Overcorrection Panic HDU/ITU-> DDAVP, 2 micrograms IV q8hr & H20
Clamp protocol:
- DDAVP (2 micrograms IV q8hr) is started immediately and continued until the sodium is close to normal.
- Sodium is corrected by infusing hypertonic solutions, primarily 3% saline. Of course, hypertonic bicarbonate. For a patient requiring volume resuscitation, a large volume of normal saline could be used as well.
- The key point is that the sodium is increased by a direct effect of the infused solutions. This differs from approaches based on treatment of the underlying problem and waiting for the kidneys to excrete free water.
- Oral fluid intake must be restricted while on DDAVP.
- Potassium supplementation should be taken into account as this is osmotically equivalent to sodium (e.g. 40 mEq KCl tablet is roughly equivalent to ~80ml of 3% NaCl).
- Medications formulated in D5W should be avoided if possible, or otherwise taken into account (e.g. 100 ml of D5W will negate the effect of ~30ml of 3% NaCl)
- If volume overload occurs, this may be managed with furosemide.
Contraindications to clamp
- Psychogenic polydipsia/excessive water intake
- Hypervolemic hyponatremia (e.g. heart failure, cirrhosis)
DDAVP dose:
SC desmopressin at 2-4 mcg every 8-12 hours or intranasal desmopressin, 20 μg, every 12 hours
The hourly urine output should decrease substantially in the first 1 to 2 hours after administration.
Urine osmolality should be checked to ensure that urine osmolality has increased; 500- to 600-mOsm/kg range = significant antiaquaretic effect.
Vaptans
Not on European guidelines, no real well established role here. no RCT and hypernatreamia/osmotic demyelination risk. Avoid.
Urea
Only in SIADH, ensure not volume deplete. A bit niche, most evidence from ITU.
- oral intake of two to three doses of 30 g of urea over 24 hours or infusion of 80 g of urea as a 30% solution over six hours, water restriction (500 mL/24 hr), and sodium supplements (120 to 360 mmole/24 hr).
- generally safe and well tolerated
- osmotic diuretic & Salt load, so main risks are overcorrection / volume depletion
58 patients at University of Pittsburgh Medical Center
Hypernatreamia
Replace H20
Free water deficit calculator. Thats basically it. No such things as pseudohypernatreamia.
To excrete concentrated water ( i.e. not loose free water and push up your Na) a medullary concentration gradiant,ADH & responsive kidney (lithium/DI etc)
Intake: drinking the ocean, hypertonic saline, primary hyperaldo
If not thirsty - hypothalamic lesion?
DI & Polyuria
In patients with polyuria, diabetes insipidus is very unlikely if urine osmolality is >700 mOsmol/kg
nephrogenic - lithium, hypercalcamia hypoK, medullary cystic disease, sickle cell, ceongentical, post obstructive
Central - trauma, surgery, invasive, booze
Give 2-4 mcg ddavp SC and monitor uOSM & vol every 30 mins for 2 hours. if Uosm increases = concentrating urine = responding = central. can be blunted due to chronic washout if longstanding ( and thus harder to coentrated due to loss of gradiant). should increment by 50% to outrule nephrogenic.
- Urine osm > 600 - concentrating ok, ?GI/other loss ? intake
- Urine osm 300-600 - partal DI. ol, CKD, post obstructive
- Urine osm = pOSM (~300) - osmotic diuresis? NB Urea is actually an effective osm in urine ( cant make it past tubular epithelium) in contrast to in the body!
- Urine osm <pOSM - DI
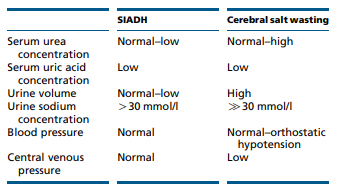
Cerebral Salt wasting
May have high urinary Cl-
Nephrogenic DI
Paradoxical role for HCTZ
- blockade of the Na-Cl cotransporter in the distal tubule leads to a decrease in GFR via Na/water secretion- > increased Na and water reabsorbotion in PT -> less delivery to CD where the concentratign issue is due to AQP issues
- May increase AQP channels and ENAC
- In Lithium induced DI , same paper showed reversal of downregulated AQP2 and increased DI
NSAIDs may help by reducing reducing the diuretic effect of renal prostaglandins
Guidelines & Protocols
Key Papers
- 22 women post uncomplicated gyne surgery - given saline / Hartmans. s[Na] dropped in 21/22.
- Hyponatremia was generally caused by generation of electrolyte-free water during excretion of hypertonic urine-a desalination process. ADH at it again.
Sodium Restriction
Evidence for restriction, especially in people with a reasonable intake is pretty weak - K+ is likely more important
Sodium-HF
low salt dietary intervention in self reportedly low intake population with limited baseline info
TLDR: poorly executed study, stopped due to futility. Probably no role for intensive dietary intervention in pateints with reasonable sodium intake.